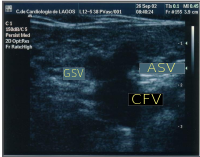
Mickey mouse signMickey Mouse signMickey Mouse sign is a medical sign resembling the head of Mickey Mouse, the Walt Disney character. Presented for the very first time at the CHIVA's Meeting, Berlin 2002 by Dr. Lurdes Cerol, this sign has been described as the image at the groin when a dilated accessory saphenous vein (ASV) exists: the common femoral vein (CFV) represents the head of Mickey Mouse while the great saphenous vein (GSV) and the dilated accessory saphenous vein (ASV) represent the ears. The presence of a Mickey Mouse sign has been a great diagnostic clue to check ASV insufficiency. Some authors, inspired by this sign, described an ecographic "Mickey Mouse View" at the saphenofemoral junction in the groin: the common femoral vein(CFV) represents the head of Mickey Mouse while the great saphenous vein (GSV) and the femoral artery (CFA) represent the ears.[1] But it can be seen in different regions of the body:
References[edit]
|
Clinicopathological findings and imaging features of intraductal papillary neoplasm of the bile duct: comparison between contrast-enhanced ultrasound and contrast-enhanced computed tomographyAbstractPurposeIntraductal papillary neoplasms of the bile duct (IPNBs) are a group of rare lesions with uncertain clinical findings and imaging features. We aim to investigate the clinicopathological features and imaging findings of IPNBs on contrast-enhanced ultrasound (CEUS) and contrast-enhanced computed tomography (CECT). MethodsFrom February 2005 to March 2018, 30 patients with pathologically confirmed IPNBs were retrospectively identified in our hospital. Demographic, clinical, and pathological data, CEUS and CECT features and surgical strategies were analyzed. ResultsThe most common clinical manifestations were abdominal pain (53.3%), jaundice (23.3%), and acute cholangitis (10.0%). Among all lesions, 5/30 (16.7%) lesions presented as dilated bile ducts only, while 13/30 (43.3%) lesions presented as dilated bile ducts with intraductal papillary masses, and 12/30 (40.0%) presented as solid masses with dilated bile ducts. For the 20 patients who underwent both CEUS and CECT, 18 lesions were hyperenhanced on CEUS, and 17 lesions were hyperenhanced on CECT in the arterial phase. In total, 16 and 18 lesions showed washout in the portal and late phases on CEUS, while the corresponding number of lesions that showed washout in the portal and late phases on CECT were 11 and 13. Twelve lesions (40.0%) showed atypical hyperplasia, while 16/30 (53.3%) lesions underwent malignant transformations. ConclusionsThere are 3 major forms of IPNBs on grayscale ultrasound, including diffusely dilated bile ducts without visible mass; focal dilated bile duct with intraductal papillary masses; and solid mass surrounded by dilated bile ducts. The enhancement patterns of IPNBs on CEUS and on CECT were consistent. IPNB has a high malignant potential, and patients should be treated with surgical resection after the diagnosis is established. |
Adrenocortical hyperplasia: a review of clinical presentation and imagingAbstractAdrenal hyperplasia is non-malignant enlargement of the adrenal glands, which is often bilateral. It can be incidental or related to indolent disease process and may be related to benign or malignant etiologies causing biochemical alterations in the hypothalamic–pituitary–adrenal axis which controls steroidogenesis and in particular cortisol production. Clinical significance of the adrenal hyperplasia is variable ranging from asymptomatic finding to serious manifestations of Cushing syndrome. This is often associated with anatomical changes in the adrenal glands, which typically manifests as diffuse and sometimes nodular enlargement of the adrenal glands radiologically. Approaching adrenal hyperplasia requires careful clinical and biochemical evaluation in correlation with imaging review to differentiate ACTH-dependent and ACTH-independent etiologies. CT is the primary modality of choice for adult adrenal imaging owing to reproducibility, temporal and spatial resolution and broader access, while MRI often serves a complimentary role. Ultrasound and MRI are most commonly used in pediatric cases to evaluate congenital adrenal hyperplasia. This article will discuss the clinical presentation and imaging features of different types and mimics of adrenal cortical hyperplasia. |
Evaluating the inflammatory activity in Crohn's disease using magnetic resonance diffusion kurtosis imagingAbstractObjectivesTo explore the feasibility of diffusion kurtosis imaging (DKI) for evaluating inflammatory activity in Crohn's disease (CD). Materials and methodsIn all, 51 CD patients were included, who were performed with consecutive enteroscopy, MR and DKI (b values = 0–2000 mm2/s). The lesions of bowel segments were graded as inactive (0–2), mild (3–6), and moderate–severe group (> 6) based on simplified endoscopic activity score for Crohn's disease (SES-CD), The abilities of the parameters of DKI and DWI in grading different activity lesions were compared. ResultsOne hundred and twenty-seven bowel segments including inactive (15), mild (45) and moderate–severe (67) were analyzed. ADC (r = − 0.627, p < 0.001), Dapp (r = − 0.381, p < 0.001) and Kapp (r = 0.641, p < 0.001) were correlated with SES-CD. These parameters were significantly different among the three groups (all p < 0.001). ROC analysis found ADC had the highest accuracy (AUC = 0.884, p < 0.001) to differentiate inactive from active group with the threshold at 0.865 × 10−3 mm2/s, which was slightly higher than Kapp (AUC = 0.867, p < 0.001) with the threshold at 0.645, and was obviously higher than Dapp (AUC = 0.726, p = 0.005). Similarly, ADC also had the highest accuracy (AUC = 0.846, p < 0.001) to differentiate inactive–mild from moderate–severe group with the threshold at 0.825 × 10−3 mm2/s, and minimally higher than Kapp (AUC = 0.843, p < 0.001) with the threshold at 0.695, and obviously higher than Dapp (AUC = 0.690, p < 0.001). ConclusionDKI is feasible and comparable to conventional DWI for the evaluation of inflammatory activity in CD. |
Magnetic resonance imaging as a non-invasive method for the assessment of pancreatic fibrosis (MINIMAP): a comprehensive study design from the consortium for the study of chronic pancreatitis, diabetes, and pancreatic cancerAbstractCharacteristic features of chronic pancreatitis (CP) may be absent on standard imaging studies. Quantitative Magnetic Resonance Imaging (MRI) techniques such as T1 mapping, extracellular volume (ECV) fraction, diffusion-weighted imaging (DWI) with apparent diffusion coefficient map (ADC), MR elastography (MRE), and T1-weighted signal intensity ratio (SIR) have shown promise for the diagnosis and grading severity of CP. However, radiologists still use the Cambridge classification which is based on traditional ductal imaging alone. There is an urgent need to develop new diagnostic criteria that incorporate both parenchymal and ductal features of CP seen by MRI/MRCP. Designed to fulfill this clinical need, we present the MINIMAP study, which was funded in September 2018 by the National Institutes of Health. This is a comprehensive quantitative MR imaging study which will be performed at multiple institutions in well-phenotyped CP patient cohorts. We hypothesize that quantitative MRI/MRCP features can serve as valuable non-invasive imaging biomarkers to detect and grade CP. We will evaluate the role of T1 relaxometry, ECV, T1-weighted gradient echo SIR, MRE, arteriovenous enhancement ratio, ADC, pancreas volume/atrophy, pancreatic fat fraction, ductal features, and pancreatic exocrine output following secretin stimulation in the assessment of CP. We will attempt to generate a multi-parametric pancreatic tissue fibrosis (PTF) scoring system. We anticipate that a quantitative scoring system may serve as a biomarker of pancreatic fibrosis; hence this imaging technique can be used in clinical practice as well as clinical trials to evaluate the efficacy of agents which may slow the progression or reverse measures of CP. |
Microvascular invasion and grading in hepatocellular carcinoma: correlation with major and ancillary features according to LIRADSAbstractPurposeTo assess major and ancillary parameters that could be correlated with Microvascular Invasion (MIV) and with histologic grade of HCC. Materials and methodsIn this retrospective study, we assessed 62 patients (14 women–48 men; mean age, 63 years; range 38–80 years) that underwent hepatic resection for HCC. All patients were subject to Multidetector computed tomography (MDCT); 40 to Magnetic Resonance (MR) study. The radiologist assessed major and ancillary features according to LIRADS (v. 2018) and reported any radiological accessory findings if detected. ResultsNo major feature showed statistically significant differences and correlation with grading. Mean ADC value was correlated with grading and with MIV status. No major feature was correlated to MIV; progressive contrast enhancement and satellite nodules showed statistically different percentages with respect to the presence of MIV, so as at the monovariate correlation analysis, satellite nodules were correlated with the presence of MIV. At multivariate regression analysis, no factor proved to be strong predictors of grading while progressive contrast enhancement and satellite nodules were significantly associated with the MIV. ConclusionMean ADC value is correlated to HCC grading and MIV status. Progressive contrast enhancement and the presence of satellite nodules are correlated to MIV status. |
Microwave ablation assisted by three-dimensional visualization system as local therapy for relapsed hepatoblastoma: a small pilot studyAbstractPurposeWe aimed to explore the feasibility of microwave ablation (MWA) assisted by three-dimensional visualization system for relapsed HB in children. MethodsFrom August 2014 to February 2017, five patients with relapsed HB were enrolled. A total of 12 liver tumors were treated with MWA assisted by a three-dimensional visualization system. Follow-up data were obtained in all patients. The residual liver volume, local tumor progression, new intrahepatic tumors, survival outcome, and complications were analyzed. ResultsAll tumors were completely ablated in a single session. The mean ablation time per tumor was 9.7 ± 8.6 min, and the median ablation/liver volume ratio was 2.37%. No local tumor progression was observed during a follow-up period of 9–39 months. All patients were still alive at the end of the follow-up. The median progression-free survival time after ablation was 9 months, and the median survival time after ablation was 12 months. No other complications were observed except for fever. ConclusionsMWA assisted by three-dimensional visualization system appears to be a safe and feasible local treatment for recurrent HB in pediatric patients. |
| The "paper-thin wall" appearance in acute mesenteric ischemia |
Demystifying the mesenteric root lesionsAbstractObjectiveThe aim of this article is to describe the normal anatomy of the root of the small bowel mesentery (RSBM) as well as the multidetector computed tomography (MDCT) features of the various primary and secondary lesions that affect the RSBM. ResultsThe small bowel mesentery attaches the jejunum and ileum to the posterior abdominal wall, the line of attachment forming the RSBM. Several primary as well as secondary lesions involve the RSBM. The RSBM has anatomical contiguity with the mesocolon and other peritoneal ligaments, which forms a route for the spread of infection, neoplasms as well as several other abdominal pathologies. MDCT plays an important role in the evaluation of mesenteric root lesions. ConclusionFamiliarity with the lesions involving the RSBM and their characteristic appearances on MDCT is important in giving thoughtful differential diagnosis and guiding the treating physician in further management. |
| Correction to: Imaging features of immune-mediated genitourinary disease The original version of this article was published with a error in the initials of the first, fifth and sixth author name: Jonathon Weber, Frank Miller and Jeanne Horowitz. The correct author's initials should be Jonathon D. Weber, Frank H Miller, and Jeanne M Horowitz. It is now corrected with this correction. |
Αρχειοθήκη ιστολογίου
-
►
2023
(256)
- ► Φεβρουαρίου (140)
- ► Ιανουαρίου (116)
-
►
2022
(1695)
- ► Δεκεμβρίου (78)
- ► Σεπτεμβρίου (142)
- ► Φεβρουαρίου (155)
-
►
2021
(5507)
- ► Δεκεμβρίου (139)
- ► Σεπτεμβρίου (333)
- ► Φεβρουαρίου (628)
-
►
2020
(1810)
- ► Δεκεμβρίου (544)
- ► Σεπτεμβρίου (32)
- ► Φεβρουαρίου (28)
-
▼
2019
(7684)
- ► Δεκεμβρίου (18)
- ► Σεπτεμβρίου (53)
-
▼
Μαΐου
(390)
-
▼
Μαΐ 15
(29)
- European Radiology
- Neuroscience
- Abdominal Radiology
- Neuroradiology
- Coloproctology
- Pharmacology and Pharmacotherapeutics
- Conservation Genetics
- Gastroenterology
- Fertility Science and Research
- Pharmacology
- Tropical Pathology
- Hematology
- Health & Allied Sciences
- Studia Logica
- Medical Humanities
- Environmental Science and Bio/Technology
- Anaesthesia
- Neurology
- Medical Journal of Dr. D.Y. Patil Vidyapeeth
- Oral Care and Research
- Environmental Radioactivity
- Palaeogeography, Palaeoclimatology, Palaeoecology
- Forensic Dental Sciences
- Clinical Practice
- Otolaryngology
- Otolaryngology–Head and Neck Surgery
- Plastic Surgery
- Physical Medicine & Rehabilitation
- Otolaryngology
-
▼
Μαΐ 15
(29)
- ► Φεβρουαρίου (2841)
- ► Ιανουαρίου (2803)
-
►
2018
(31838)
- ► Δεκεμβρίου (2810)
- ► Σεπτεμβρίου (2870)
- ► Φεβρουαρίου (2420)
- ► Ιανουαρίου (2395)
-
►
2017
(31987)
- ► Δεκεμβρίου (2460)
- ► Σεπτεμβρίου (2605)
- ► Φεβρουαρίου (2785)
- ► Ιανουαρίου (2830)
-
►
2016
(5308)
- ► Δεκεμβρίου (2118)
- ► Σεπτεμβρίου (877)
- ► Φεβρουαρίου (41)
- ► Ιανουαρίου (39)
Αλέξανδρος Γ. Σφακιανάκης
ΩτοΡινοΛαρυγγολόγος
Αναπαύσεως 5
Άγιος Νικόλαος Κρήτη 72100
2841026182
6032607174
Τετάρτη 15 Μαΐου 2019
Abdominal Radiology
Εγγραφή σε:
Σχόλια ανάρτησης (Atom)

Δεν υπάρχουν σχόλια:
Δημοσίευση σχολίου